Excretion and osmoregulation
The process of elimination or removal of harmful
substances from the body is known as excretion.
The organs associated with the removal of harmful substances known as excretory system. Major excretory system is urinary system because most of the
nitrogenous waste products, excess water and other toxic substances are thrown
outside as urine. Skin, lungs liver and intestine are known as accessory excretory organs. Nitrogenous
waste products are eliminated by urinary
system (kidney).Volatile substances
(alcohol, water vapour) are eliminated by lungs. Skin removes salts, water and
fat derivatives.
Excretory
products in animals
On the basis of nitrogenous waste products animals are
classified as;
Characters
|
Ammonotelism
|
Urotelism
|
Uricotelism
|
Nitrogenous waste
|
Ammonia
|
Urea
|
Uric acid
|
Habit
|
Aquatic
|
Aquatic/semiaquatic/terresrial
|
Terrestrial
|
Examples
|
Protista, invertebrates, fresh
water fish and larva of amphibians
|
Cartilage fish, marine bony
fish, adultamphibian semiaquatic reptiles and all mammals.
|
Terrestrial insects, mollusks,
land reptiles and all birds.
|
Excretory
system of man
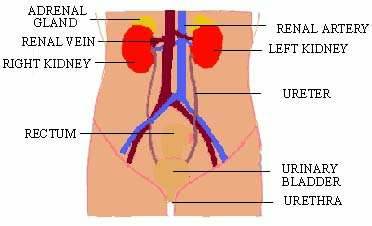
Excretory system of human are-1.Apair of kidney
2.Apair of ureter 3.Urinary bladder 4.Urethra
Kidneys
Each kidney is dark red bean
shaped measured about 11cm long and
150gm weight. They either side of vertebral column of lumber region. Right
kidney is slightly lower than left. Each kidney is enclosed by renal fascia, adipose capsule and renal capsule. Blood vessels, Lymph
vessels, nerves and ureter enter or leave from hilus renalis of kidney.
Microscopic
structure of kidney
Histologically, each kidney is composed of about one million nephrons.
L.S. of kidney shows two distinct regions-
1. Cortex:
It is outer dark part of kidney. It consists of Bowmann’scapsule and nephrons.
2. Medulla: Medulla
is made up of conical modularly pyramids (15-16).Between the pyramids cortex
extends as renal column of bertini. These
modularly pyramid are connected with minor
calyces then major calyces. The
calyces open into renal pelvis.
Ureters
These
are one pair. Ureters are thin and muscular tube of about 30 cm long. These
arise from hilum of kidney and open in to urinary bladder. Upper portion is renal pelvis and lower is ureter proper.
Urinary bladder
It is thin muscular elastic bag
located in abdominal cavity. Longitudinal fibers and circular fibers make the
bag expanding. The collection of urine in bladder and discharging time from urethra is called micturition. Internal
sphincter and external sphincter
(voluntary) control the micturition.
Internally,
the bladder has a triangular area called
trigone in which three openings are opened. Two are openings of ureters one is opening
of ureters and one is opening of urethra. A urinary bladder can collect about
300ml urine.
Urethra
It is
a short canal. Its length is 20 cm long in male and 4cm in female. It is called
urinogenital duct in male as it serves for passage of urine and semen.
Structure of a
Nephron (Uriniferous tubule)
Nephrons
are the structural and functional units of kidney. These are about one million
(ten lakh) uriniferous tubules or nephrons in kidney. Nephron differentiated
into:
- Malpighian body
- Renal tubule
- Malpighian body: It has a cup like Bowman’s capsule and a network of blood capillaries called glomerulus. Bowman’s capsule is a small double walled cup. Outer layer is parietal and inner layer is visceral. Visceral cells form passage of fluid to filtrate in to Bowman’s capsule.
Glomerulus
is a blood capillary network in Bowman’s capsule. Entering is afferent renal arteriole and exists as efferent arteriole. Afferent lumen is
wider than arteriole. The capillaries have small pores of about 100A0diameter.
- Renal tubule: It is coiled tubular located behind the Bowman’s capsule. It has following parts:
i.
Proximal
convoluted tubule (PCT): Internally it is lined with brush bordered
cuboidal epithelium. It increases the surface area for absorption. Mitochondria
provide the energy for active absorption. It is located in cortex and
responsible for reabsorption.
ii.
Henle’s loop:
It is middle U-shaped. It lies in the medulla. It has thin descending limb and a thick ascending
limb. Both limbs are supplied with parallel capillary system called vasa recta. These supply nutrient and
carry reabsorbed water away.
iii.
Distal
convoluted tubule (DCT): It is posterior part and located in cortex. It
maintains the concentration of urine.
iv.
Collecting duct
(CD): The DCT opens in to collecting tubule. It is present in the medulla
region. The collecting tubule joins to form large Ducts of Bellini and to Renal pelvis. These ducts drain all the
urine towards the pelvis.
About 85% nephrons lie in cortex (cortical nephrons) they don’t have vasa
rectae. About 15% of total nephrons lie in medulla (juxtamedullary nephrons).These are highly supplied with vasa
rectae.
Mechanism of
Excretion or Urine Formation
These
are three steps:
1. Ultrafiltration
2. selective
reabsoption
3. Tubular
secretion
Ultrafiltration (Glomerular filtration)
It is the first process of urine
formation. It takes place in the glomerulus. Richards (1942) explained, the dissolved substances are filtered
out in to the Bowmen’s capsule due to the pressure of blood.
The
afferent arteriole enters the glomerulus and exist the form of efferent
arteriole. The useful and harmful substances are filtered in Bowmen’s capsule.
These are glucose, amino acids, vitamins and harmful substances---nitrogenous
wastes (like uric acid, ammonia, creatine, large amount of salts) etc. These
are the low molecular weight substances. Large molecules like protein, fats, and
carbohydrates are not filtered.
The
diameter of afferent arteriole is wider than diameter of efferent arteriole. So
that more blood enters into the glomerulus and less blood volume exists. Which
create hydrostatic pressure of blood
in capillaries and force tend to move fluid out of the glomerulus. It is called
ultra filtration.
1. The
hydrostatic pressure of blood (Pb) in the afferent arteriole is about 70mmHg.
2. Opposing
pressure against the hydrostatic pressure are- pressure of plasma proteins (Po)
= -30mmHg, Fluid in side
the renal tubule = -10mmHg, and pressure of intestinal fluid (Pi) = -10mmHg.Total pressure for glomerular filtration
(GFP) = 70-(30+10+10) =70-50=20mmHg.The GFP (20mmHg) is the net filtration
pressure responsible for filtration of large amount of water, different useful
and harmful substances flowing in blood.
About 180 liters of fluid are
filtered from plasma but only about 11/2litre of urine is produced
every day.
Selective Reabsorption
This is the second
step in urine formation. It takes place in PCT and Henle Loop. PCT posses many
brush bordered microvilli for absorption of filtrate. Mitochondria present it
provide the energy for active absorption.
When the filtrate
flows through PCT all useful substances are selectively absorbed from the
filtrate to the blood capillaries by both passive and active transport
mechanisms.
About 50% of urea
in the filtrate diffuses back in blood capillaries by diffusion and about 80%
of water by osmosis. Then much reduced volume of filtrate passes into Henle’s
loop.
FIG:showing selective absorption and tubular secretion
FIG:showing selective absorption and tubular secretion
Tubular Secretion
It is the final
step in urine formation. It takes place in distal convoluted and collecting.
When tubular flows through the distal convoluted tubule(DCT) unwanted
substances present in the blood such as uric acid, hippuric acid creatine,
ammonia, K+ and H+ are secreted by the blood in to the
tubular fluid by the process of active transport. At the same time, Na, Cl, and
Ca are moved from the urine into blood to regulate the concentration of ions in
plasma. Water also reabsorbed or secreted in the DCT according to the need of
water by the body. The regulation of water is controlled by antidiuretic hormone (ADH) released
from posterior pituitary gland.
Counter Current Mechanism
The two limbs of
Henle loops are opposite in property and the flow of filtrate is opposite in
direction. This process is Counter
Current Mechanism. The mechanism concentrates the urine due to the water diffusion. Vasa rectae are the veins present in
between the limbs, act as counter current exchangers. The endothelial lining of
vasa rectae is freely permeable to ions, urea and water. Role of Henle’s loop and
Role of vasa rectae are important for Counter
Current Mechanism.
Descending limb of the loop of Henle is
fully permeable to water but slightly permeable to Na+ and Cl-.The wall of Ascending limb is largely impermeable
to water but fully permeable to Na+ and Cl-.
As the filtrate
passes through the descending limb of Henle loop, water moves out in the
interstitial fluid (the fluid between vasa rectae and loop) and to the vasa
rectae. The phenomenon maintains the high concentration of solutes in the in
interstitial fluid. In the ascending limb Na+ from the filtrate and
Cl- pass out passively. Concentrations of NaCl become high in
interstitial fluid, deep in medulla and lowest in cortex. The ions draw out
water from descending limb and from collecting duct. The ions move out from the
ascending limb, the filtrate becomes progressively hypotonic(less
concentrated).
Composition of Urine
a. About 96% water
b. Urea
2%
c. Urochrome,
urinod, uric acid, creatine, K+, H+ phosphates, Oxalates
etc are 2-3%.Urochrome makes the
urine yellow colour and urinod gives
bad smell to urine.
Isotonic urine is the concentration of water in urine=
concentration of water in blood plasma.
Hypotonic urine is the concentration of water in urine >
concentration of water in blood plasma.
Hypertonic urine is the concentration of water in urine<
concentration of water in blood plasma.
Q. Write differences between
descending limb and ascending limb of Henle loop, PCT and DCT, Tubular reabsoption
and Tubular secretion.
Osmoregulation
by kidney
Osmoregulation is the maintenance of constant osmotic condition to regulate the water
content and solute concentration in body.
1. Osmoregulation in bony fishes (freshwater)
The fresh
water bony fishes have gills and kidney for the osmoregulation. The fishes have
gills and kidney for the osmoregulation. The fishes have hypertonic body
fluids. Therefore there is a constant loss of ions from body. It balances the
volume of water and salts by three means;
a. Produce large amount of glomerular filtrate
b. The large amount of selectively reabsorbed
solute passes through the renal tube so fish excrete hypotonic urine.
c. Freshwater fish can take up Sodium ion and
Chlorine ion from water directly due to the patience of Ionocytes cells in
their gills.
2. Osmoregulation in marine bony fishes: The
fishes have hypotonic body fluid. There is constant loss of water from body.
Marine fish conserve the water and loss ion to overcome dehydration of tissue
by following ways:
a. It constantly drinks sea water. Kidney lack
of glomeruli so nitrogenous wastages are secreted directly into renal tubules
and water is absorbed by osmosis.
b. Ionocytes help to expel monovalent anions
from body fluids to seawater and divalent cations from faeces.
3. Osmoregulation in human: In case of human hypertonic urine is excreted. This minimizes the water loss from their body. The filtrate
fluid in Bowman's capsule (isotonic) passes through the tubules of nephrones.
Then a large amount of water and solutes are reabsorbed during this course.
During cold month, hypotonic urine is excreted but in warmer month
hypertonic urine is excreted due to sweating.
ADH and regulation of water reasbsorption
Antidiuretic hormone (ADH) or vasopressin is the hormone
released by posterior part of pituitary gland. The main function of ADH is to
increase permeability of distal convoluted tubule (DCT) and collecting duct
(CD) due to which reabsorption of water increases. There are two conditions to
balance water:
1. When a person takes small amount of water: In this condition large amount of salt is
ingested in diet or excessive sweating then solute potential of the body fluids
become more negative (Osmotic pressure rises in the blood). The change in the
osmotic potential is detected by osmoreceptors in the hypothalamus and carried
to the brain. The brain detects such changes in the body and pituitatory gland
releases ADH in the blood.
A large amount of water is reabsorbed rapidly from the filtrate into the
cortex and medulla and passes back into the blood capillaries to maintain
osmotic pressure normal. So that urine becomes highly concentrated and reduced
volume of urine is released from kidney. It is generally called anti-diuresis.
2. When a person takes large amount of water: When a person takes large amount of water or
little sweating or extremely low salt intake in diet then the solid potential
of the blood becomes less negative. (Osmotic pressure becomes low in blood)
This condition is detected by osmoreceptors and carried to the brain. It sends
the message to the pituitary gland to inhabit the
In absence of ADH walls of DCT and CD are impermeable to water and less
water is reabsorbed as the osmotic pressure of filtrate is normal and large
volume of diluted urine is excreted. It is generally called diuresis.
The regulation
of water by ADH is an example of
homeostatic feedback mechanism.
Other functions of kidney
1.
Regulation of fluid balance: The kidney
controls osmotic pressure of extra cellular body fluids by regulating the
amount of water lost from body.
2.
Regulation of electrolyte concentrations: The
concentration of electrolytes like Sodium, Potassium, Chloride Bicarbonates etc
in blood also regulated. It is performed by selective tubular
reasbsorption process in proximal tubule.
3.
Maintenance of acid-base balance
4.
Removal of other substances like mineral salts,
iodides, drugs, arsenic and bacteria are recovered of the blood by kidney only.
5.
Kidney secretes rennin which is an enzyme
but acts as hormone which changes the plasma protein.
6.
Kidney secretes erythropoietin which stimulates
the formation of RBC.
Functions of skin
1. Barrier against the invasion of microorganism
and chemicals
2. Regulate the dehydration
3. Barrier against UV light
4. Regulate the body temperature
5. Acts as to regulate excretion of some
substances
6. Absorption of some substances
7. Sensitivity in response to stimuli
Functions of
liver (consult from previous chapter digestive system)
1. Deamination: Body is unable to store excess
amino acids which are deaminated in the liver. Amino acids are oxidized by
oxygen to release acid and amino group. The removal of amino group (-NH2)
from amino acid is called deamination. Structural formula………..
2. Detoxification: The toxic ammonia is
converted into less toxic compound urea. It takes place in liver. This occurs
by cyclic reaction known as ornithine cycle. In this process two molecules of
ammonia combined with one molecule of carbon dioxide to form Urea and water.
Homeostasis
The regulation or maintenance of a constant body fluid
or internal environment is called homeostasis. The temperature, amount of water
and glucose concentration are at almost constant in homeostasis. At the
temperature of 37 oC enzymes work perfectly, division of cell and
metabolism is also perfect.
The term homeostasis was first put forward by French
biologist Claude Bernard in 1859. In
1929, American physiologist Walter
Cannon first used the term homeostasis and studied about it. Homeostatic
organs are skin, liver, kidney lungs, endocrine glands etc.
- Skin as homeostatic organ: Skin helps in temperature regulation. It possesses pigment cells (chromatophores and melanophores), sweat glands and sebaceous glands which help in controlling the heat and fluid balance. The melanin pigment helps to absorb solar heat and increase body temperature.
- Kidney as homeostatic organ: Kidneys are the chief excretory and osmoregulatory organs. These also play key role in homeostasis. For example, (a) Regulation of water content by ADH (b) Regulation of salt or ion concentration in blood (c) Maintain acid base balance in body (Lactic acid, ketones, sulphuric acid etc) (d) Blood volume is regulated by the kidney
- Liver as homeostatic organ: Liver is a key homeostatic organ due to the following reasons: (a) Regulation of Carbohydrate, lipid and amino acid metabolism. (b) Regulation of amount of glucose in blood by gluconeogenesis process. (c) It maintains the optimum temperature (d) Liver produces the bile. Bilirubin and Biliverdin, by products of dead RVC are excreted from the liver.
- Lungs as homeostatic organ: It balances the concentration of O2 and Co2 in blood at the best level for the cells’ chemical reaction.






Best ias coaching in bangalore
ReplyDelete.www.globalias.in